What Makes People Feel “Dizzy?”
When people report feeling dizzy, it may mean several different things. “Dizziness” is a term that describes several broad types of symptoms:
- Vertigo – a false sensation of movement, especially of whirling, spinning, or being off-balance.
- Lightheadedness – sometimes referred to as “presyncope” (syncope means fainting), this is a feeling of being about to faint.
- Disequilibrium – this is a sensation of being unsteady or off-balance that is brought on by visual illusions or other dysfunctions in the visual system of the eyes and brain.
- Psychological dizziness – a variety of symptoms brought on by anxiety or other psychological disorders, often described as a feeling of floating, rocking back and forth, or being removed from one’s body.

All types of dizziness are a serious concern, as they can cause falls and other accidents. People who suddenly become dizzy while driving may lose control of their vehicle and cause a motor vehicle accident.
Besides the significant safety risk, dizziness has been associated with depressive symptoms, worsened self-reported health, and reduced overall well-being.
Does COVID-19 Cause People to Feel Dizzy?
The first two types of dizziness – vertigo and lightheadedness – have been associated with COVID-19 infection. The virus that causes COVID-19 (the “severe acute respiratory syndrome coronavirus 2” or “SARS-CoV-2” virus) can bring on dizziness in a variety of ways, some of which are not yet fully understood. COVID-19 has hit humankind hard and fast, and still presents many unanswered questions to medical science.
People who are already prone to falls – such as the elderly – may be especially susceptible to suffer injury from dizziness. Unfortunately, this is the same population that is most susceptible to experience moderate to severe symptoms when infected with COVID-19.
Let’s look at each of these two types of dizziness and how they are related to COVID-19.
Vertigo and COVID-19
Vertigo has recently been identified as a symptom of COVID-19. In fact, about 2% of people who become infected with SARS-CoV-2 will experience vertigo as their first symptom.
Vertigo is a disturbing and even dangerous symptom. Although vertigo itself is a sensation of spinning, swaying, and being off-balance, it’s usually also accompanied by nausea and vomiting, visual disturbances, and sweating. These accompanying symptoms may be severe. The dizziness, nausea, vomiting, and sweating usually appear suddenly – as if out of nowhere – and can cause people to fall from their feet, or lose the ability to control their vehicle if they’re driving.
Bouts of vertigo can come and go, lasting anywhere from seconds to hours, or they can be constant, lasting days or weeks. Vertigo can be debilitating. People are often so off-balance that they cannot even stand or walk. Even laying in bed with vertigo is uncomfortable, as the world seems to be spinning around. They are often unable to read or even watch TV in many cases because of the whirling sensation and visual disturbances. As well, the nausea and vomiting can be severe, worsening the experience.
Vertigo can be caused by anything that affects the body’s mechanisms for maintaining our sense of balance. COVID-19 can cause vertigo by disrupting the balance circuits in the brain and the inner ear.
Vertigo that is caused by disruption of the brain’s balance circuits is known as “central vertigo,” because it involves the brain, which is part of the central nervous system. The brain circuits involved in our sense of balance are primarily in the brainstem and cerebellum.
COVID-19, like many other viruses, is known to be “neuroinvasive,” which means that it is able to get into the brain and cause disease. The research literature has documented that about 36% of people with COVID-19 develop neurological symptoms from the effects of the SARS-CoV-2 virus on the brain.
The SARS-CoV-2 virus – which causes COVID-19 – has been found to cause brain swelling, partial brain cell degeneration, and brain inflammation (“encephalitis”). It seems to primarily do so through its activation of the immune system, which produces chemicals (“cytokines”) that can be toxic to the brain.
In addition to these mechanisms of injuring the brain, the virus can also cause a stroke. This can occur due to inadequate oxygen supply to the brain due to impaired lung function. As well, COVID-19 is known to cause an increase in blood clotting, which can result in blood clots travelling in the bloodstream and blocking the brain’s circulation. In these ways, COVID-19 makes infected patients susceptible to stroke, even if the virus doesn’t make it to the brain.
If any of these mechanisms of injuring the brain occur in the areas responsible for the sense of balance, vertigo may occur. As well, when COVID-19 affects the brain, other symptoms may be present, such as headache, confusion, visual disturbances, and impaired sense of smell.
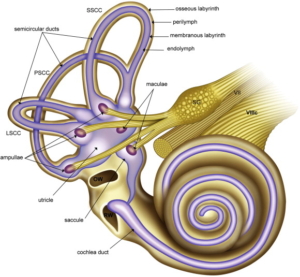
In addition to central vertigo – caused by brain dysfunction – vertigo can also be caused by inner ear problems; in which case it is known as “peripheral vertigo.” The inner ear contains the vestibular apparatus, which is an anatomical structure that senses whether or not we are moving or tilted. Anything that disturbs the vestibular apparatus can cause vertigo by fooling the brain into thinking that we are off-balance or moving.
COVID-19 can induce peripheral vertigo by causing inflammation of the vestibular nerve (“vestibular neuritis”), inflammation of the vestibular apparatus itself (“labyrinthitis”), or by causing inflammation of the nearby middle ear (“otitis media”).
The specific nature of the vertigo symptoms – such as how long the bouts of vertigo last, whether or not the vertigo is continuous, and the severity of the vertigo – depend upon which part of the balance system is affected. For example, central vertigo may produce different symptoms than will labyrinthitis or vestibular neuritis. This helps doctors and physical therapists assess where the cause of the dizziness is and how best to treat it.
Lightheadedness and COVID-19
As with vertigo, people who experience lightheadedness – the feeling of being about to faint – often describe the symptom as dizziness or being dizzy.
Lightheadedness is caused by an inadequate oxygen supply to the brain. It usually resolves rapidly as soon as the brain gets enough oxygen again, but fainting, coma, and even death may occur if adequate oxygen supply is not promptly restored.
Inadequate oxygen intake and circulation is a common manifestation of severe COVID-19. People with severe cases of COVID-19 may require a breathing life support system (intubation and ventilation) in an ICU until they recover from the infection.
COVID-19 can cause lightheadedness in several ways:
- Inadequate lung function – COVID-19 causes pneumonia (inflammation of the lungs), which can cause serious impairment of lung function. As well, COVID-19 can cause the part of the brain that controls breathing to malfunction, so that the body stops trying to breathe.
- Heart problems – even if the lungs and breathing are working properly, inadequate circulation due to heart problems can result in inadequate oxygenated blood getting to the brain. COVID-19 has been associated with several heart problems that can significantly affect circulation:
- Heart attack or angina (myocardial ischemia), Inflammation of the heart (myocarditis), and
Irregular heartbeat (arrhythmia),Blood clots – COVID-19 is known to cause excessive clotting of the blood (“hypercoagulability”). This can result in blood clots that travel in the bloodstream (“thromboembolism”) and cause injury to the lungs, heart, or brain, and
- Low blood pressure (“hypotension”) – COVID-19 has been associated with sudden, extreme drops in blood pressure that can cause impaired circulation and oxygenation of vital body tissues, including the brain.
- Lightheadedness (presyncope) and/or fainting (syncope) have been reported to occur in about 3% of COVID-19 cases. Most cases are older people (the average age in one study was 69), and those with other health problems, especially heart disease, diabetes, and high blood pressure.
COVID-19 Dizziness and Vertigo
Of the two types of dizziness symptoms associated with COVID-19 – vertigo and lightheadedness – vertigo is generally the most problematic and severe. Lightheadedness is usually transient and resolves as soon as oxygen supply is restored; often even lying down and elevating the feet (the “Trendelenburg” position) is all that’s required.
Vertigo, however, tends to be much longer lasting, and difficult to treat. Unlike lightheadedness, the cause of vertigo dizziness is often difficult to discover, and difficult to treat. At this point, it’s unclear how long dizziness symptoms will continue in people who develop COID-19-associated vertigo, simply because we don’t have enough long-term data available. Some causes of vertigo are associated with chronic dizziness, but we do not yet know if this occurs with COVID-19.
Treating Vertigo Dizziness
Unfortunately, dizziness from vertigo is difficult to treat, and there are no medications that very effective at relieving the horrible dizziness. Medications are used to try to reduce swelling in the inner ear or brain (such as steroids, diuretics, and antihistamines), and to treat nausea. Unfortunately, many of these medications are very sedating, and do not provide much relief from the dizziness.
Hopefully, treating the COVID-19 and allowing the body to heal from the effects of the virus will likely result in the resolution of the vertigo, but we don’t yet know for sure what to expect.
A type of physical therapy known as “vestibular rehabilitation” offers a non-medication approach to relieving dizziness from vertigo. Some cases of dizziness from vertigo may not get better unless the individual is treated with specific exercises and physical therapy for their dizziness and balance.
Audiologists and physical therapists are trained to assess each patient’s dizzy symptoms in order to customize the optimal treatment approach for that individual’s specific type of vertigo. This is important because different types of vertigo respond to different types of treatment. This is why expertise in treating vertigo is important when selecting a physical therapist.
Vestibular rehabilitation exercises may include walking exercises, head and eye exercises, and balance exercises. As well, physical therapists can provide education about the specifics of the dizziness, and important safety information.
With vestibular rehabilitation, audiologist and physical therapists are able to achieve several specific goals for improving vertigo dizziness and stabilizing balance and gait. This involves using several therapeutic principles that are well known to improve postural control and balance:
Adaptation – this involves training individuals with the symptoms of dizziness to overcome the false perception of movement due to errant signals from the inner ears to the eyes to the brain, spine, and feet.
Habituation – this is where physical therapists introduce repetitive movements that are designed to get the brain used to moving properly despite the vertigo. With repetition, the brain gets used to (habituates to) the vertigo and begins ignoring the false signals from the balance system, and
Sensory substitution – this involves strengthening other senses, specifically vision and sense of touch (“proprioception”), in order to compensate for the impaired sense of balance.
A recently published systematic review of the research literature has shown that exercise-based vestibular rehabilitation provides significant improvements in vertigo symptoms, balance, and the emotional effects of dealing with dizziness, as well as reducing the risk of falls from dizziness.
Dizziness Treatment
Hearing & Balance Centers provide specialized physical therapy for a wide variety of musculoskeletal, neurological, and inner ear conditions that cause dizziness and poor balance, including vertigo.
The dizziness treatment program uses established proprietary treatment and recovery protocols that include specialized cutting-edge equipment that is not available at other physical therapy centers. This makes the specialized physical therapists an excellent choice for those seeking relief from dizziness of any kind.
We concentrates on strengthening the impaired vestibular system and engaging “neuroplasticity” – the ability of the brain to learn new movements and behaviors – to optimize other senses (such as vision and touch) to compensate for the brain’s or inner ear’s inability to maintain a proper sense of balance. This optimizes adaptation, habituation, and sensory substitution for helping get dizzy patients back on their feet and functioning again.
Article courtesy of FYZICAL