Preserving Auditory and Vestibular Health: A Comprehensive Guide to Hearing and Balance Care
Abstract:
The auditory and vestibular systems are vital for communication, spatial orientation, and overall functional independence. Dysfunction in these systems contributes to substantial health burdens, including social isolation, cognitive decline, and heightened fall risk. This paper reviews evidence-based strategies for preserving hearing and balance across the lifespan, encompassing environmental, behavioral, and clinical interventions aligned with current audiological guidelines.
1. Introduction
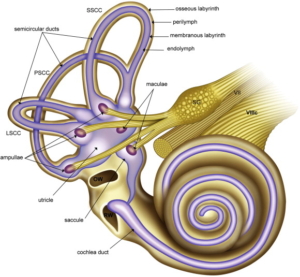
The human ear serves dual functions: sound perception and balance regulation. The cochlea mediates auditory transduction, while the semicircular canals and otolith organs govern equilibrium. Damage or degeneration within these systems can significantly impair quality of life. With global population ageing, the preservation of hearing and balance has become a critical public health priority.
2. Anatomy and Physiology
- Auditory system: The external, middle, and inner ear structures work in concert to facilitate the mechanical and neural transmission of sound.
- Vestibular system: The semicircular canals, utricle, and saccule, in coordination with visual and proprioceptive inputs, maintain postural stability and gaze control.

3. Risk Factors for Dysfunction
- Noise exposure: Prolonged or excessive noise can result in noise-induced hearing loss (NIHL).
- Ototoxic medications: Agents such as aminoglycosides, cisplatin, and loop diuretics may damage cochlear and vestibular hair cells.
- Age-related changes: Presbycusis and vestibular decline contribute to sensory deficits in older adults.
- Systemic conditions: Diabetes, cardiovascular disease, and autoimmune disorders can compromise auditory and vestibular function.
4. Strategies for Hearing Health
- Hearing protection: Use of earplugs or earmuffs in hazardous noise environments; adherence to safe listening practices (e.g., 60/60 rule).
- Routine monitoring: Periodic audiological assessments for at-risk individuals, including industrial workers and older adults.
- Ototoxicity surveillance: Baseline and serial audiometry during administration of ototoxic therapies.
- Infection prevention: Vaccination and appropriate management of otitis media and meningitis to reduce the risk of sensorineural hearing loss.
5. Strategies for Balance Health
- Vestibular rehabilitation: Gaze stabilization, habituation, and balance training to promote central compensation.
- Fall prevention: Home safety modifications, strength and gait training in vulnerable populations.
- Lifestyle measures: Adequate hydration, and dietary adjustments (e.g., low-sodium diet in Meniere’s disease).
- Sensory support: Regular vision checks and proprioceptive exercises to enhance multisensory integration.
6. Interdisciplinary and Technological Approaches
- Amplification and implants: Hearing aids and cochlear implants to improve auditory function and reduce cognitive load.
- Assistive devices: Use of mobility aids and wearable sensors to support balance.
- Tele-audiology: Expanding access to hearing and balance care in underserved regions.
- Public health initiatives: Community education on hearing conservation and fall risk reduction.
7. Clinical Recommendations
- Incorporate hearing and balance screening into routine health assessments.
- Provide counselling on modifiable lifestyle factors affecting auditory and vestibular health.
- Ensure timely referral to audiologists, ENT specialists, or vestibular therapists for early intervention.
8. Conclusion
The preservation of auditory and vestibular function is fundamental to maintaining independence and well-being. Audiologists play a central role in delivering preventive care, early diagnosis, and tailored interventions. Ongoing research and public health strategies are essential to meet the evolving needs in hearing and balance health.
References
(Suggested: peer-reviewed literature, WHO guidelines, CDC publications, “Audiology: Science to Practice,” “Balance Function Assessment and Management.”)
The Editor of this article is Richard Mwangi, a Consultant Audiologist at Doctors Of Hearing- Kenya

